- Hypothalamus and pituitary gland
- Clinical Characteristics, Diagnosis, and Treatment of Thyroid Stimulating Hormone-Secreting Pituitary Neuroendocrine Tumor (TSH PitNET): A Single-Center Experience
-
Jung Heo, Yeon-Lim Suh, Se Hoon Kim, Doo-Sik Kong, Do-Hyun Nam, Won-Jae Lee, Sung Tae Kim, Sang Duk Hong, Sujin Ryu, You-Bin Lee, Gyuri Kim, Sang-Man Jin, Jae Hyeon Kim, Kyu Yeon Hur
-
Endocrinol Metab. 2024;39(2):387-396. Published online February 5, 2024
-
DOI: https://doi.org/10.3803/EnM.2023.1877
-
-
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material PubReader PubReader  ePub ePub
- Background
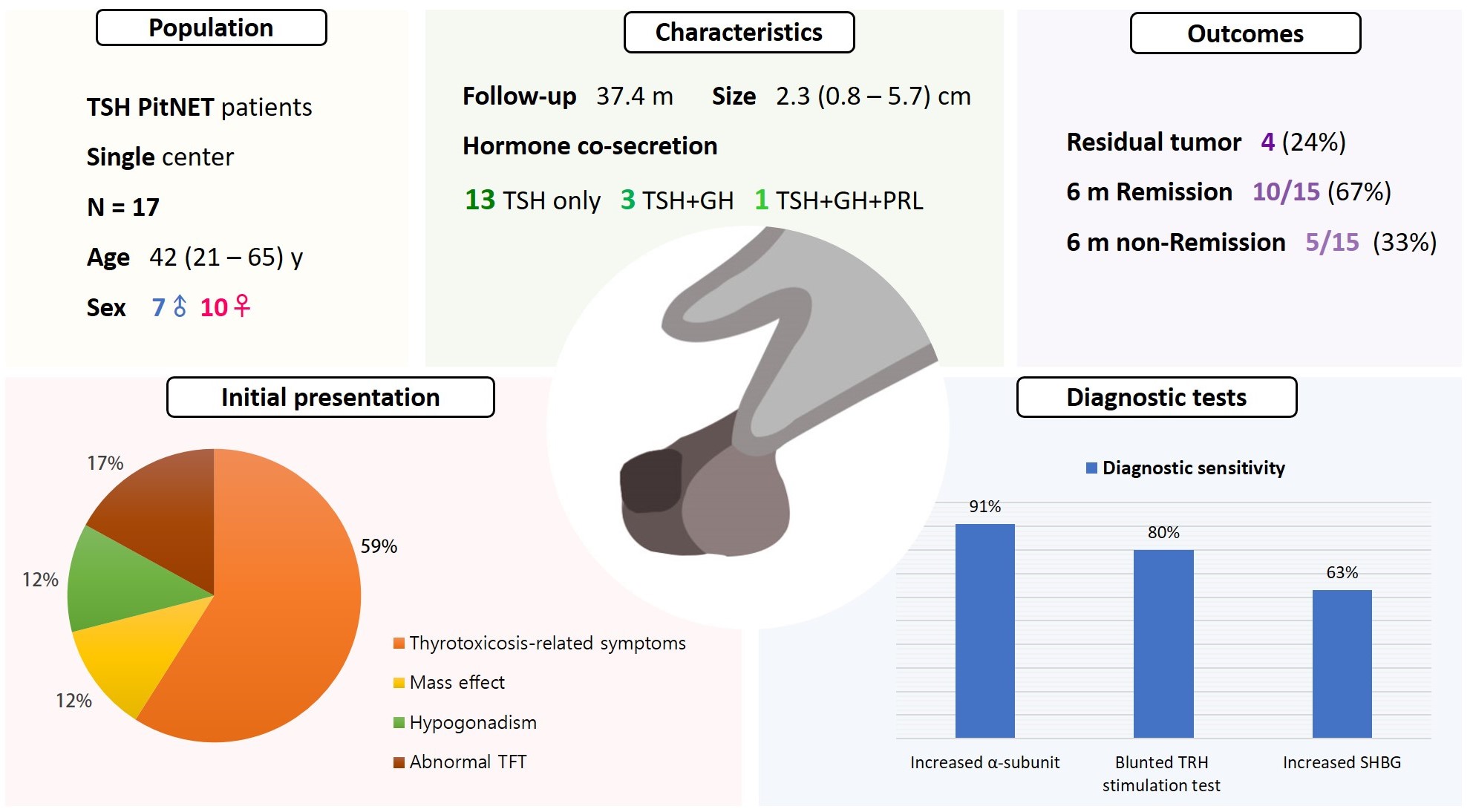
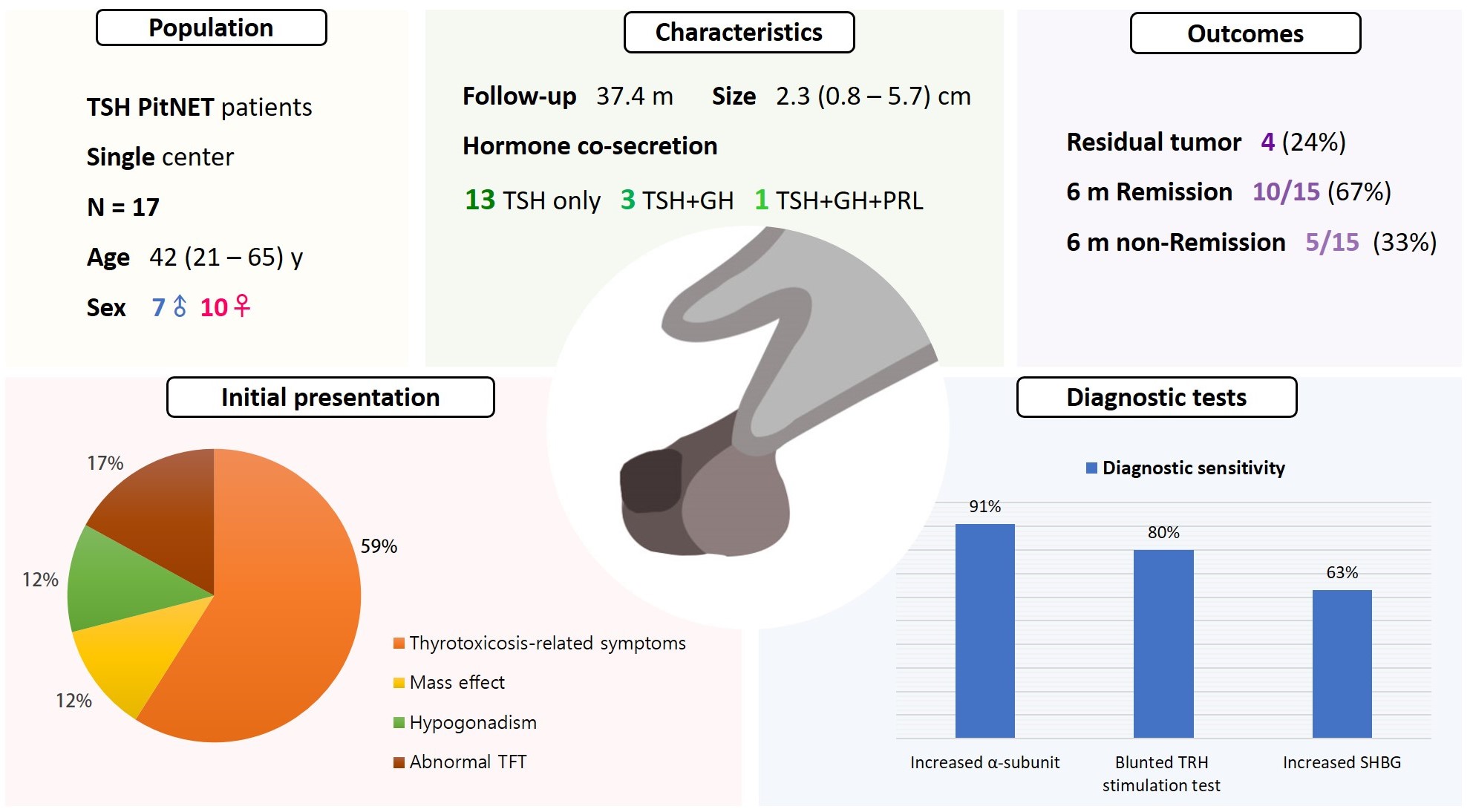
Thyroid-stimulating hormone (TSH)-secreting pituitary neuroendocrine tumor (TSH PitNET) is a rare subtype of PitNET. We investigated the comprehensive characteristics and outcomes of TSH PitNET cases from a single medical center. Also, we compared diagnostic methods to determine which showed superior sensitivity.
Methods
A total of 17 patients diagnosed with TSH PitNET after surgery between 2002 and 2022 in Samsung Medical Center was retrospectively reviewed. Data on comprehensive characteristics and treatment outcomes were collected. The sensitivities of diagnostic methods were compared.
Results
Seven were male (41%), and the median age at diagnosis was 42 years (range, 21 to 65); the median follow-up duration was 37.4 months. The most common (59%) initial presentation was hyperthyroidism-related symptoms. Hormonal co-secretion was present in four (23%) patients. Elevated serum alpha-subunit (α-SU) showed the greatest diagnostic sensitivity (91%), followed by blunted response at thyrotropin-releasing hormone (TRH) stimulation (80%) and elevated sex hormone binding globulin (63%). Fourteen (82%) patients had macroadenoma, and a specimen of one patient with heavy calcification was negative for TSH. Among 15 patients who were followed up for more than 6 months, 10 (67%) achieved hormonal and structural remission within 6 months postoperatively. A case of growth hormone (GH)/TSH/prolactin (PRL) co-secreting mixed gangliocytoma-pituitary adenoma (MGPA) was discovered.
Conclusion
The majority of the TSH PitNET cases was macroadenoma, and 23% showed hormone co-secretion. A rare case of GH/TSH/PRL co-secreting MGPA was discovered. Serum α-SU and TRH stimulation tests showed great diagnostic sensitivity. Careful consideration is needed in diagnosing TSH PitNET. Achieving remission requires complete tumor resection. In case of nonremission, radiotherapy or medical therapy can improve the long-term remission rate.
- Adrenal Gland
- Aldosterone Immunoassay-Specific Cutoff Value for Seated Saline Suppression Test for Diagnosing Primary Aldosteronism
-
So Yoon Kwon, Jiyun Park, So Hee Park, So Hyun Cho, You-Bin Lee, Soo-Youn Lee, Jae Hyeon Kim
-
Endocrinol Metab. 2022;37(6):938-942. Published online December 6, 2022
-
DOI: https://doi.org/10.3803/EnM.2022.1535
-
-
1,772
View
-
194
Download
-
1
Web of Science
-
1
Crossref
-
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material PubReader PubReader  ePub ePub
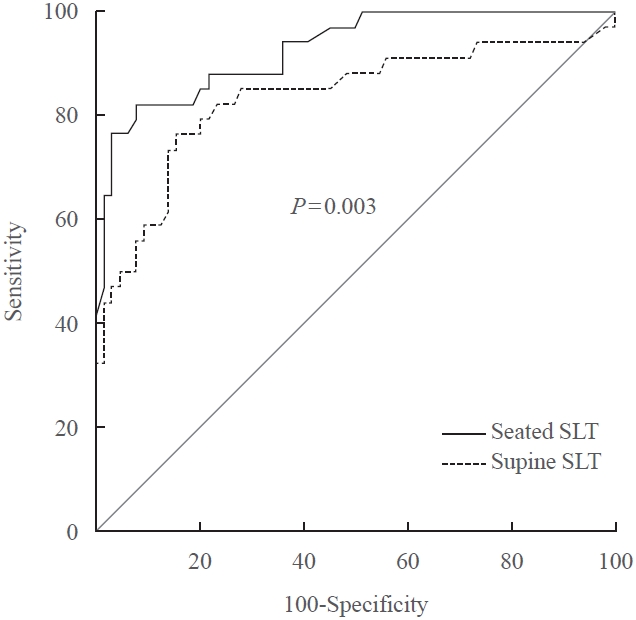
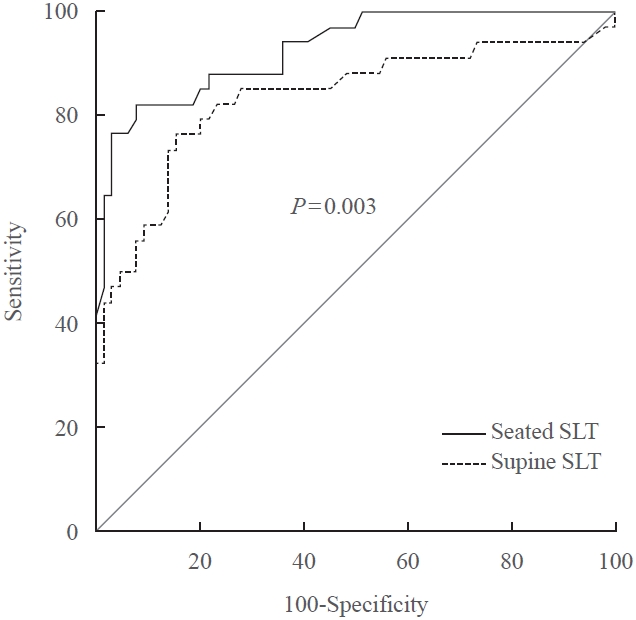
- A seated saline loading test (SLT) using liquid chromatography-tandem mass spectrometry (LC-MS/MS) is one of the most accepted confirmatory tests of primary aldosteronism. However, LC-MS/MS is time-consuming and is not widely available in diagnostic laboratories compared to immunoassay. With immunoassay, it is unknown whether SLT in the seated position is more accurate than that of the supine position, and a cutoff value of post-seated SLT plasma aldosterone concentration (PAC) must be established in the Korean population. Ninety-eight patients underwent SLT in both positions, and post-SLT PAC was measured by LC-MS/MS and radioimmunoassay. We confirmed primary aldosteronism if post-seated SLT PAC by LC-MS/MS exceeded 5.8 ng/dL. The area under the receiver operating characteristic curve was greater for seated than supine SLT (0.928 vs. 0.834, P=0.003). The optimal cutoff value of post-seated SLT by radioimmunoassay was 6.6 ng/dL (sensitivity 83.3%, specificity 92.2%).
-
Citations
Citations to this article as recorded by  - Investigating the cut-off values of captopril challenge test for primary aldosteronism using the novel chemiluminescent enzyme immunoassay method: a retrospective cohort study
Yuta Tezuka, Kei Omata, Yoshikiyo Ono, Kengo Kambara, Hiroki Kamada, Sota Oguro, Yuto Yamazaki, Celso E. Gomez-Sanchez, Akihiro Ito, Hironobu Sasano, Kei Takase, Tetsuhiro Tanaka, Hideki Katagiri, Fumitoshi Satoh
Hypertension Research.2024;[Epub] CrossRef
- Adrenal gland
- Diagnosis for Pheochromocytoma and Paraganglioma: A Joint Position Statement of the Korean Pheochromocytoma and Paraganglioma Task Force
-
Eu Jeong Ku, Kyoung Jin Kim, Jung Hee Kim, Mi Kyung Kim, Chang Ho Ahn, Kyung Ae Lee, Seung Hun Lee, You-Bin Lee, Kyeong Hye Park, Yun Mi Choi, Namki Hong, A Ram Hong, Sang-Wook Kang, Byung Kwan Park, Moon-Woo Seong, Myungshin Kim, Kyeong Cheon Jung, Chan Kwon Jung, Young Seok Cho, Jin Chul Paeng, Jae Hyeon Kim, Ohk-Hyun Ryu, Yumie Rhee, Chong Hwa Kim, Eun Jig Lee
-
Endocrinol Metab. 2021;36(2):322-338. Published online April 6, 2021
-
DOI: https://doi.org/10.3803/EnM.2020.908
-
-
7,505
View
-
572
Download
-
8
Web of Science
-
10
Crossref
-
 Abstract Abstract
 PDF PDF PubReader PubReader  ePub ePub
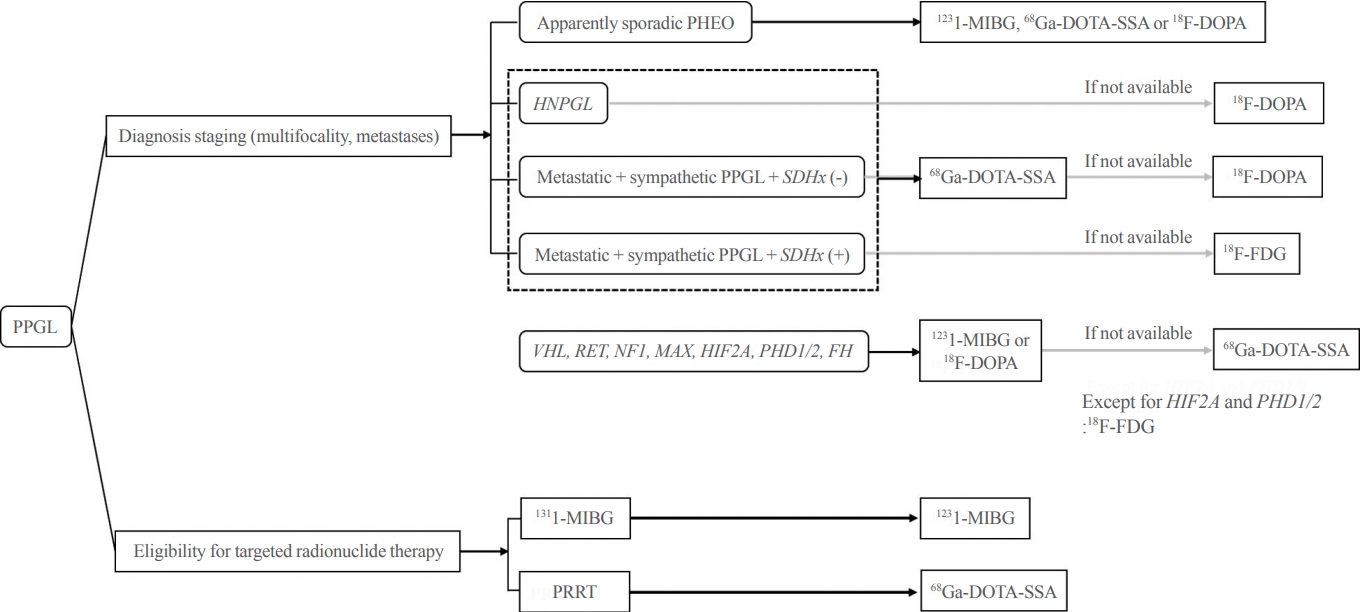
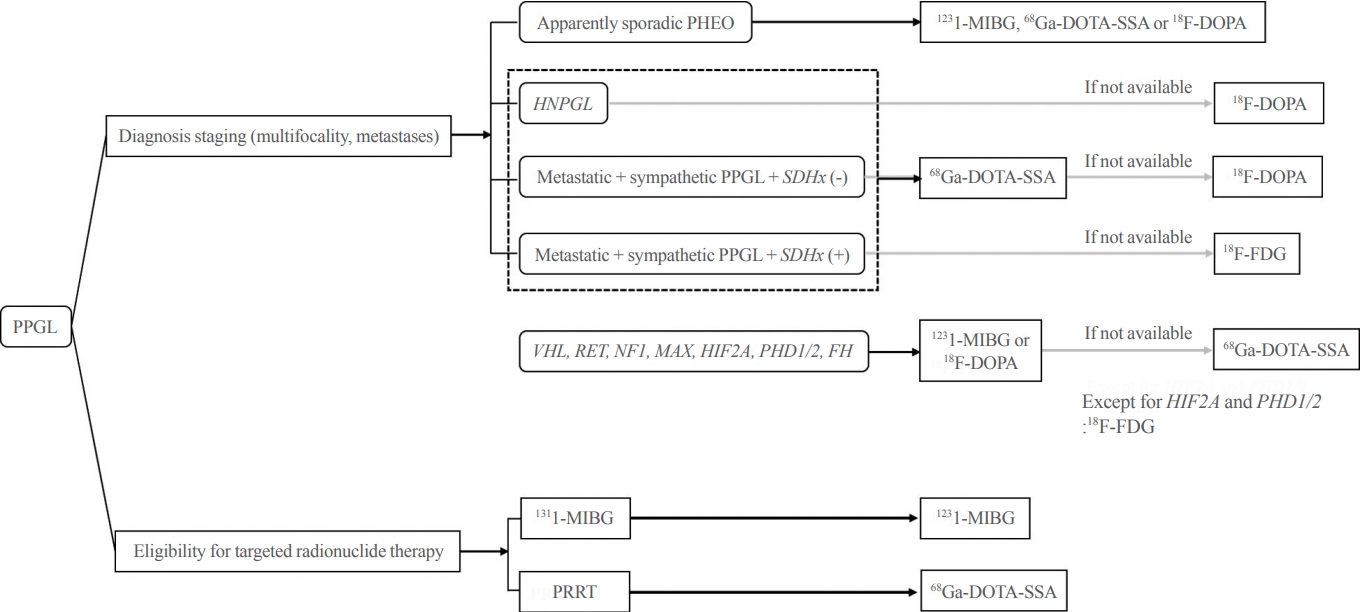
- Pheochromocytoma and paraganglioma (PPGLs) are rare catecholamine-secreting neuroendocrine tumors but can be life-threatening. Although most PPGLs are benign, approximately 10% have metastatic potential. Approximately 40% cases are reported as harboring germline mutations. Therefore, timely and accurate diagnosis of PPGLs is crucial. For more than 130 years, clinical, molecular, biochemical, radiological, and pathological investigations have been rapidly advanced in the field of PPGLs. However, performing diagnostic studies to localize lesions and detect metastatic potential can be still challenging and complicated. Furthermore, great progress on genetics has shifted the paradigm of genetic testing of PPGLs. The Korean PPGL task force team consisting of the Korean Endocrine Society, the Korean Surgical Society, the Korean Society of Nuclear Medicine, the Korean Society of Pathologists, and the Korean Society of Laboratory Medicine has developed this position statement focusing on the comprehensive and updated diagnosis for PPGLs.
-
Citations
Citations to this article as recorded by  - A Prospective Comparative Study of 18F-FDOPA PET/CT Versus 123I-MIBG Scintigraphy With SPECT/CT for the Diagnosis of Pheochromocytoma and Paraganglioma
Changhwan Sung, Hyo Sang Lee, Dong Yun Lee, Yong-il Kim, Jae Eun Kim, Sang Ju Lee, Seung Jun Oh, Tae-Yon Sung, Yu-Mi Lee, Young Hoon Kim, Beom-Jun Kim, Jung-Min Koh, Seung Hun Lee, Jin-Sook Ryu
Clinical Nuclear Medicine.2024; 49(1): 27. CrossRef - Evaluation and Management of Bone Health in Patients with Thyroid Diseases: A Position Statement of the Korean Thyroid Association
A Ram Hong, Ho-Cheol Kang
Endocrinology and Metabolism.2023; 38(2): 175. CrossRef - Lesion-based indicators predict long-term outcomes of pheochromocytoma and paraganglioma– SIZEPASS
Helena Hanschell, Salvador Diaz-Cano, Alfredo Blanes, Nadia Talat, Gabriele Galatá, Simon Aylwin, Klaus Martin Schulte
Frontiers in Endocrinology.2023;[Epub] CrossRef - Interleukin-6-producing paraganglioma as a rare cause of systemic inflammatory response syndrome: a case report
Yin Young Lee, Seung Min Chung
Journal of Yeungnam Medical Science.2023; 40(4): 435. CrossRef - (Extremely rare intrapericardial location of paraganglioma)
Jaroslav Zajíc, Aleš Mokráček, Ladislav Pešl, Jiří Haniš, Dita Schaffelhoferová
Cor et Vasa.2023; 65(4): 692. CrossRef - A Case of Von Hippel-Lindau Disease With Recurrence of Paraganglioma and No Other Associated Symptoms: The Importance of Genetic Testing and Establishing Follow-Up Policies
Naoki Okada, Akihiro Shioya, Sumihito Togi, Hiroki Ura, Yo Niida
Cureus.2023;[Epub] CrossRef - KSNM60 in Nuclear Endocrinology: from the Beginning to the Future
Chae Moon Hong, Young Jin Jeong, Hae Won Kim, Byeong-Cheol Ahn
Nuclear Medicine and Molecular Imaging.2022; 56(1): 17. CrossRef - Change of Computed Tomography-Based Body Composition after Adrenalectomy in Patients with Pheochromocytoma
Yousun Ko, Heeryoel Jeong, Seungwoo Khang, Jeongjin Lee, Kyung Won Kim, Beom-Jun Kim
Cancers.2022; 14(8): 1967. CrossRef - Evaluation and Management of Bone Health in Patients with Thyroid Diseases: a Position Statement from the Korean Thyroid Association
A Ram Hong, Hwa Young Ahn, Bu Kyung Kim, Seong Hee Ahn, So Young Park, Min-Hee Kim, Jeongmin Lee, Sun Wook Cho, Ho-Cheol Kang
International Journal of Thyroidology.2022; 15(1): 1. CrossRef - Pheochromocytoma with Retroperitoneal Metastasis: A Case Report
建新 崔
Advances in Clinical Medicine.2021; 11(05): 2239. CrossRef
- Adrenal gland
- Bilateral Adrenocortical Masses Producing Aldosterone and Cortisol Independently
-
Seung-Eun Lee, Jae Hyeon Kim, You-Bin Lee, Hyeri Seok, In Seub Shin, Yeong Hee Eun, Jung-Han Kim, Young Lyun Oh
-
Endocrinol Metab. 2015;30(4):607-613. Published online December 31, 2015
-
DOI: https://doi.org/10.3803/EnM.2015.30.4.607
-
-
4,121
View
-
46
Download
-
5
Web of Science
-
4
Crossref
-
 Abstract Abstract
 PDF PDF PubReader PubReader
A 31-year-old woman was referred to our hospital with symptoms of hypertension and bilateral adrenocortical masses with no feature of Cushing syndrome. The serum aldosterone/renin ratio was elevated and the saline loading test showed no suppression of the plasma aldosterone level, consistent with a diagnosis of primary hyperaldosteronism. Overnight and low-dose dexamethasone suppression tests showed no suppression of serum cortisol, indicating a secondary diagnosis of subclinical Cushing syndrome. Adrenal vein sampling during the low-dose dexamethasone suppression test demonstrated excess secretion of cortisol from the left adrenal mass. A partial right adrenalectomy was performed, resulting in normalization of blood pressure, hypokalemia, and high aldosterone level, implying that the right adrenal mass was the main cause of the hyperaldosteronism. A total adrenalectomy for the left adrenal mass was later performed, resulting in a normalization of cortisol level. The final diagnosis was bilateral adrenocortical adenomas, which were secreting aldosterone and cortisol independently. This case is the first report of a concurrent cortisol-producing left adrenal adenoma and an aldosterone-producing right adrenal adenoma in Korea, as demonstrated by adrenal vein sampling and sequential removal of adrenal masses. -
Citations
Citations to this article as recorded by  - Different cell compositions and a novel somatic KCNJ5 variant found in a patient with bilateral adrenocortical adenomas secreting aldosterone and cortisol
Liling Zhao, Jinjing Wan, Yujun Wang, Wenjun Yang, Qi Liang, Jinrong Wang, Ping Jin
Frontiers in Endocrinology.2023;[Epub] CrossRef - Adrenal Vein Cortisol to Metanephrine Ratio for Localizing ACTH-Independent Cortisol-Producing Adenoma: A Case Report
Rishi Raj, Philip A Kern, Neelima Ghanta, Edilfavia M Uy, Kamyar Asadipooya
Journal of the Endocrine Society.2021;[Epub] CrossRef - Adrenal Venous Sampling for Subtype Diagnosis of Primary Hyperaldosteronism
Mitsuhide Naruse, Akiyo Tanabe, Koichi Yamamoto, Hiromi Rakugi, Mitsuhiro Kometani, Takashi Yoneda, Hiroki Kobayashi, Masanori Abe, Youichi Ohno, Nobuya Inagaki, Shoichiro Izawa, Masakatsu Sone
Endocrinology and Metabolism.2021; 36(5): 965. CrossRef - Hypercortisolism and primary aldosteronism caused by bilateral adrenocortical adenomas: a case report
Kaiyun Ren, Jia Wei, Qilin Liu, Yuchun Zhu, Nianwei Wu, Ying Tang, Qianrui Li, Qianying Zhang, Yerong Yu, Zhenmei An, Jing Chen, Jianwei Li
BMC Endocrine Disorders.2019;[Epub] CrossRef
|